The project outlined below was selected to receive a 2019 Community Service Award from the AHNS Cancer Prevention Service. In conjunction with Oral Head & Neck Cancer Awareness Week which takes place in April each year, AHNS annually gives out five $1000 awards for projects related to cancer prevention. For more information about the 2020 awards and application, please click HERE.
Benjamin M. Laitman, MD, PhD; Mingyang Liu Gray, MD, MPH; Brett A, Miles, DDS, MD – Department of Otolaryngology Head and Neck Surgery, Icahn School of Medicine at Mount Sinai, New York
It is essential for physicians to be well-educated sources of information for their patients. According to the CDC, 44,430 new cases of head and neck cancers (HNC) were reported in 2015, resulting in 9,754 deaths in the US. Importantly, 70-90% of newly diagnosed HNCs are Human papilloma virus (HPV)- induced1,2, an incidence which has increased in the United States by 225% from 1988-2004. Most of the newly diagnosed HPV+ cancers would be preventable with the HPV vaccine3. However, only 65.5% of US teens have initiated, and only 48.6% were up to date with, the HPV vaccine series as of 20174. Physicians are uniquely influential, as strong vaccine recommendations have been linked to increased HPV vaccine uptake and intent to vaccinate5,6. Therefore, knowledge of the association between HPV infection and HNC is an essential tool when counseling the parents of vaccine-eligible children.
Unfortunately, work we have done to assess physician knowledge of HPV+ HNC is discouraging7. In a national assessment of knowledge of HPV’s association with HNC in 3141 medical students and residents, we found that only ~50% of medical students correctly identified associations between persistent HPV infection HNC, a level that surprisingly did not increase throughout residency. Furthermore, when counseling on the vaccine, residents only discussed HNC as a potential outcome of the disease only 40% of the time, attributing this practice to a lack of knowledge on the subject.
Such results are not surprising, as ENT training, including the head and neck exam, is poorly represented in medical education8. Especially those students pursuing primary care specialties report poorer overall comfort managing ENT problems, leading to missed diagnoses and delay in proper treatment. Thus, interventions to train primary care physicians (PCPs) on the HNC exam have the potential to increase provider likelihood of properly examining patients and improving HNC identification9.
Such improved screening in high-risk populations can reduce morbidity and mortality due to HNC10. Studies have shown that certain populations, including African Americans and Hispanics have disproportionate rates of HNC morbidity and mortality 10-12, likely due to a combination of implicit bias and limited access to care. Residents at Mount Sinai Hospital, situated in East Harlem in NYC, have the opportunity to treat a large number of those individuals impacted by this lack of care. East Harlem has a high rate un-insured residents (12%) in New York City 13. In a population of 124,323 people, approximately one quarter (24%) are foreign born, 50% are Hispanic and 30% black. Importantly, 23% of residents live below the poverty level and 14% reported going without needed medical care13.
It is clear, with such gaps in knowledge and skills in PCPs, that those with the greatest proficiency in HNC work-up and management (otolaryngologists) must educate other health-care providers so we all can adequately prevent and detect HNC, especially in high-risk communities such as our own.
The grant from AHNS allowed our team to create and conduct workshops to educate primary care providers in internal medicine and pediatrics on the importance of HNC screening, HPV vaccination, as well as on general head and neck anatomy knowledge. Using supplies funded by the AHNS we conducted 1-hour long hands-on, interactive workshops during the afternoon didactics for pediatric and internal medicine residency programs at the Mount Sinai Hospital. The workshops consisted of a 10-minute introduction on the prevention, detection, and early workup of HNC. Following this, participants divided into 4 groups to conduct 5-7 minute hands-on learning activities including discussions of (1) HPV vaccination on preventing certain HNCs and (2) risk factors for various HNC cancers, (3) performing the head and neck physical exam, and (4) working thorough clinical case scenarios for the initial management of patients that may have a new primary HNC. After completing all workshops, participants reconvened for a summary of key points.
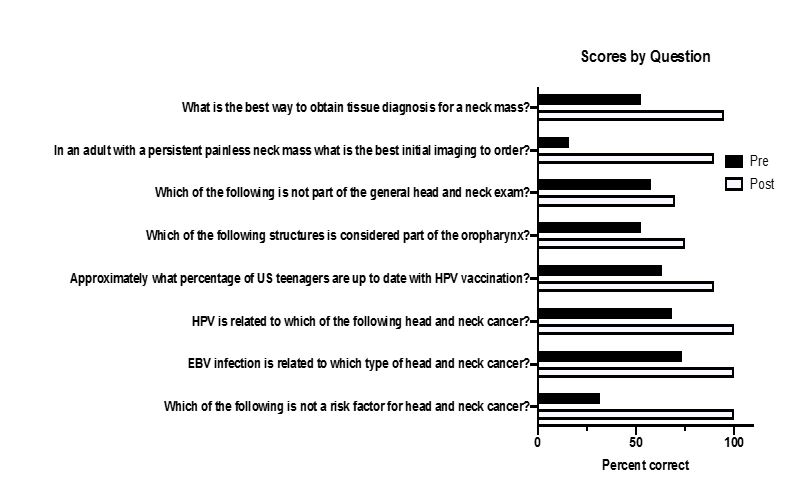
We assessed effectiveness of these sessions by having participants take pre- and post-workshop surveys evaluating knowledge of HPV vaccines, HNC identification, work-up, and management and comfort with the head and neck exam and oral cancer screening. 11 pediatrics residents and 8 internal medicine residents participated and completed surveys; 5 were in their first year of residency, 8 were PGY2’s, and 9 were PGY3’s. Eight multiple choice knowledge questions were asked pertaining to the focus of the introductory didactic and 4 workshop stations. Participants answered 50% of questions correctly on pre-surveys, with correct responses increasing significantly to 90% after the workshop (see Figure below for scores on individual questions).
Improving knowledge and skills in only a handful of PCPs has the ability to impact thousands of patients over the course of these physicians’ careers. Instead of providing a screenings/education for a small subset of patients, we hope instead to have provided the knowledge and tools for physicians to prevent and detect cancers for years to come. It is our plan to continue this workshop annually and expand it to residency programs throughout the institution.
Figure legend (please click image to enlarge text): Graph shows the percentage of participants who correctly answered knowledge question on pre- and post-surveys. Significant increases were seen in the percentage of correct responses for each knowledge question.
References
- Chaturvedi AK, Engels EA, Pfeiffer RM, et al. Human papillomavirus and rising oropharyngeal cancer incidence in the United States. Journal of Clinical Oncology. 2011;29(32):4294-4301.
- Deschler DG, Richmon JD, Khariwala SS, Ferris RL, Wang MB. The “New” Head and Neck Cancer Patient—Young, Nonsmoker, Nondrinker, and HPV Positive:Evaluation. Otolaryngology–Head and Neck Surgery. 2014;151(3):375-380.
- Centers for Disease Control and Prevention. 6 Reasons to get HPV vaccine for your child. https://www.cdc.gov/hpv/infographics/vacc-six-reasons.html. Accessed October 26, 2018.
- Walker TY, Elam-Evans LD, Yankey D, et al. National, Regional, State, and Selected Local Area Vaccination Coverage Among Adolescents Aged 13-17 Years – United States, 2017. MMWR Morb. Mortal. Wkly. Rep. Vol 672018:909-917.
- Mohammed KA, Vivian E, Loux TM, Arnold LD. Factors Associated With Parents' Intent to Vaccinate Adolescents for Human Papillomavirus: Findings From the 2014 National Immunization Survey-Teen. Prev Chronic Dis. Vol 142017:E45.
- Brewer NT, Hall ME, Malo TL, Gilkey MB, Quinn B, Lathren C. Announcements Versus Conversations to Improve HPV Vaccination Coverage: A Randomized Trial. Pediatrics. Vol 1392017.
- Laitman BM, Ronner, L., Oliver, K., Genden, E. U.S. Medical Trainees’ Knowledge of Human Papilloma Virus and Head and Neck Cancer. Otolaryngology-Head and Neck Surgery. 2019;In press.
- Fung K. Otolaryngology–head and neck surgery in undergraduate medical education: advances and innovations. Laryngoscope. Vol 125 Suppl 2: John Wiley & Sons, Ltd; 2015:S1-14.
- Wee AG, Zimmerman LM, Anderson JR, et al. Promoting oral cancer examinations to medical primary care providers: a cluster randomized trial. J Public Health Dent. Vol 762016:340-349.
- Iyer S, Thankappan K, Balasubramanian D. Early detection of oral cancers: current status and future prospects. Curr Opin Otolaryngol Head Neck Surg. Vol 242016:110-114.
- Moore CE, Warren R, Maclin SD. Head and neck cancer disparity in underserved communities: probable causes and the ethics involved. J Health Care Poor Underserved. Vol 232012:88-103.
- Daraei P, Moore CE. Racial Disparity Among the Head and Neck Cancer Population. J Cancer Educ. Vol 30: Springer US; 2015:546-551.
- Hinterland KN, M; King, L; Lewin, V; Myerson, G; Noumbissi, B; Woodward, M; Gould, LH; Gwynn, RC; Barbot, O; Bassett, MT. Manhattan Community District 11: East Harlem. Community Health Profiles 2018. 2018;11(59):1-20.




 AHNS Receives Highest CME Designation
AHNS Receives Highest CME Designation