AHNS – What’s New on the Website – September 2023
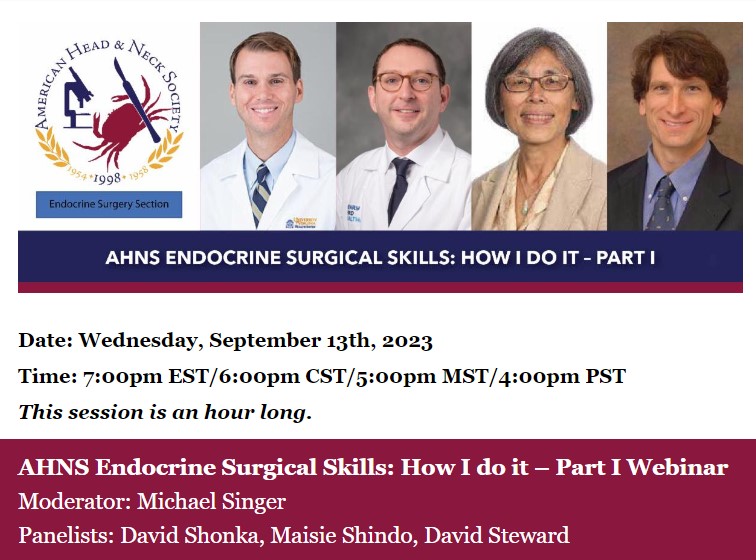
New Content on the AHNS Website Click on the highlighted links below to see What’s New from AHNS! NEW – A Message from Laura Jackson, PhD – AHNS Myers’ Family Summer Travel Fellowship in Otolaryngology Diversity 2023 Winner presented by Mentor Dr. Lisa Shnayder and the AHNS Diversity Service NEW – AHNS Dr. Eddie Méndez Fellowship …