Authored by Nilesh Vasan, MD & Arjun Joshi, MD; edited by Miriam Lango, MD
AHNS Education Committee
What is a Neck Dissection and Why is it Performed?
Neck dissection is usually performed to remove cancer that has spread to lymph nodes in the neck.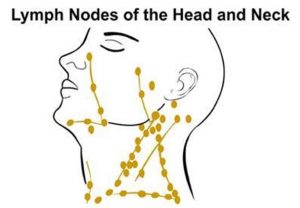
Lymph nodes are small bean shaped glands scattered throughout the body that filter and process lymph fluid from other organs. The immune cells in the lymph nodes help the body fight infection. When cancer cells spread from another part of the body, they may get caught in a lymph node where they grow. An individual might feel a non-tender lump in the neck. The cancer in the lymph node is known as a metastasis. When someone undergoes surgery for cancer that has spread to lymph nodes, both the initial or primary cancer as well as the metastases must be removed.
Neck dissection refers to the removal of lymph nodes and surrounding tissue from the neck for the purpose of cancer treatment. The extent of tissue removal depends on many factors including, the stage of disease which reflects the extent of cancer as well as the type of cancer. The most common cancers removed from lymph nodes in the neck include head and neck squamous cell carcinomas, skin cancers including melanoma and thyroid cancers.. In general, the goal of neck dissection is to remove all the lymph nodes within a predefined anatomic area. Many of the lymph nodes removed during surgery will not prove to have cancer in them.
 Many patients wonder why so many non-cancerous lymph nodes must be removed; why can’t surgery be done to remove only the lymph nodes with cancer in them?
Many patients wonder why so many non-cancerous lymph nodes must be removed; why can’t surgery be done to remove only the lymph nodes with cancer in them?
A cancer may shed any number of metastases that lodge in lymph nodes, grow and spread. There are over 150 lymph nodes on each side of the neck. During an operation, a surgeon will not be able to tell if a lymph node is clean, or if it has cancer that will later grow into a visible neck lump. The lymph nodes must be processed and tested; this takes time. For that reason, it is recommended that the lymph nodes in a predefined region are removed, not just lymph nodes that are obviously enlarged with cancer.
In addition, different cancers spread differently. Skin cancers first spread to lymph nodes in different parts of the neck than thyroid cancers or oral or larynx cancers. Squamous cell carcinomas that start in the lining or mucosa of the mouth, throat or larynx have a tendency to spread to lymph nodes early; cancer cells can often be detected in lymph nodes in the neck when examined under the microscope, even in the absence of visible or palpable neck lumps.
Lymph node metastasis reduces the survival of patients with squamous cell carcinoma by half. The survival rate is less than 5% in patients who previously underwent surgery and have a recurrent metastasis in the neck. Therefore, the control of cancer that has spread to the neck is one of the most important aspects in the successful management of these particular cancers. The neck dissection is a standardized procedure that was developed to ensure the complete removal of cancer that has spread to the lymph nodes of the neck.
Radical vs. Modified Neck Dissection
Radical Neck Dissection
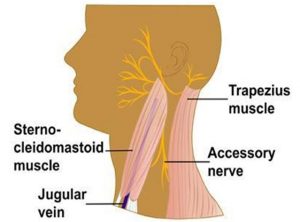
- This operation has been used for almost 100 years and describes the removal of lateral neck nodes and tissues to surgically remove cancer in the neck. Included in this tissue, which extends from the collarbone (clavicle) inferiorly to the jawbone (mandible) superiorly are dozens of lymph nodes. In addition to lymph nodes, this operation often includes remove the submandibular gland (a saliva-producing gland in the upper neck), the sternocleidomastoid muscle, the jugular vein and the spinal accessory nerve (to the trapezius muscle).
- The radical neck dissection was designed to ensure complete cancer removal in individuals with very advanced cancers in the neck. The radical neck dissection is effective but produces characteristic cosmetic changes. Because so much tissue is removed, one side of the neck may appear flatter than the other. More importantly, sacrifice of the nerve to the trapezius muscle results in visible drooping of the shoulder and difficulty in raising the arm over head. Some individuals develop pain in the neck and collarbone. An intensive physical therapy program may diminish some of these problems, but some long-term disability can be anticipated.
Historically, radical neck dissections were the most commonly performed type of neck dissection performed by surgeons. This is no longer the case. Most patients are candidates for a less radical operation.
Modified Radical Neck Dissection
- This term describes a variety of neck dissections that preserve structures that are usually sacrificed in the radical neck dissection such as the spinal accessory nerve, the internal jugular vein or sternocleidomastoid muscle. Further, selective neck dissections are neck dissections that, in addition to preserving these important structures, are used to remove specific groups of lymph nodes, rather than all the lymph nodes on the side of the neck, based on the probability that those lymph nodes harbor cancer.
- While radical neck dissections produce the greatest changes in cosmetic appearance and shoulder function, selective neck dissections produce the least. In fact, selective neck dissections frequently produce no obvious cosmetic changes, yielding a nearly invisible scar. Nevertheless, strength and flexibility may be enhanced with adherence to neck and shoulder range of motion exercises after surgery. The best results can be expected with faithful adherence to an exercise program over the long term.
The Procedure
Neck dissections are done under general anesthesia through an incision that runs along a skin crease in the neck, extending vertically on the side of the neck. Incisions are usually designed to enhance the visualization and protection of important structures in the neck, and enable the safe removal of lymph nodes that harbor cancer.
Beneath the skin, underlying fat, and a thin layer of muscle (the platysma), the dissection proceeds to identify and remove the tissue containing the lymph nodes. If the sternocleidomastoid muscle is removed as part of the operation, there may be some flattening of the neck, but removal of this muscle rarely results in significant weakness.
What are the risks of neck dissection?
Neck dissections are subject to numerous potential operative complications that are common to all operative procedures, as well as complications specific to this procedure. Some of these are described below, but do not include all potential complications associated with neck dissection. The risk of specific complications may be best determined for an individual by the nature and extent of their cancer, prior treatment and other circumstances.
- Bleeding-Patients may bleed after an operation. Bleeding under the skin after a neck dissection is rare. Sometimes an operative procedure to remove the blood is required. Rarely, a blood transfusion is also needed.
- Infection can occur after any surgical procedure including neck dissection (uncommon)
- Chyle leak, which results in fluid accumulation in the neck from disruption of the thoracic duct (this problem is more common after left sided neck dissections) (rare)
- Wound healing problems requiring additional surgery (rare)
Several important nerves are found in the neck around the lymph nodes, and depending on the area of the neck to be operated, these nerves can be at risk for damage. The primary nerves of concern are-
- The marginal nerve, a small branch of the facial nerve which controls lower lip movement
- The spinal accessory nerve which aids in shoulder mobility and raising the arm over head
- The hypoglossal nerve, which controls movement of the tongue (uncommon)
- The lingual nerve, which controls sensation on the side of the tongue (rare)
- The vagus nerve which controls movement of one vocal cord (rare)
Additional potential long-term problems include:
- Incision-Most incisions heal well, but some individuals develop scars.
- Numbness of the skin along the incision as well as over the cheek, ear and neck can be anticipated which improves with time; some long term numbness can be anticipated
- Neck stiffness or pain
- Long term swelling in the neck or lymphedema
- Shoulder weakness (uncommon)
- Changes in speech and swallowing (rare)
Some problems are attributable to nerve injury; more commonly, scarring under the skin from surgery and radiation contributes to disability. Some problems may be avoided with early and faithful adherence to a shoulder range of motion exercise program, lymphedema or speech therapy rehabilitation programs.
