Introduction to Skin Cancer
Welcome to the AHNS Cutaneous Cancer Section Patient Information pages. This webpage serves as an introduction to skin cancer in the head and neck region. Skin cancer can be especially distressing when it occurs on the head, face or neck as this is the most visible part of your body. Treatment of cancers of this area requires detailed attention to the nearby structures including nerves and muscles underlying the skin. This will help to preserve the aesthetic outcome and the unique functions of this area. If you or your loved one has developed skin cancer of the head, face or neck, you can follow this link to search for a surgeon nearby who specializes in treating these cancers.
We hope this content will help you find the information you need about head and neck skin cancers.
Developed by the AHNS Cutaneous Cancer Section, Patient Education Subcommittee
Alice Lin, MD; Karen Choi, MD; Kevin Emerick, MD; Mirabelle Sajisevi, MD
Introduction to the Disease
Basal Cell Carcinoma
Squamous Cell Carcinoma
Cutaneous Malignant Melanoma
Merkel Cell Carcinoma
Sebaceous Cell Carcinoma
Diagnosis of Skin Cancers
Treatment
Clinical Trials
Survivorship
Skin Cancer Prevention
Surveillance for Skin Cancer
*******************************************************************
Introduction to the Disease
- Skin cancer is a malignant growth on the skin. It is also the most common type of cancer.
- The majority of skin cancers can be treated effectively or “cured” with surgery to remove the cancer.
- Once you have developed a skin cancer, it is important to follow up with your doctor and routinely check for new cancers.
Basal Cell Carcinoma
Article by Karen Choi, MD
 Basal cell carcinoma (BCC) is the most common skin cancer and usually develops in sun-exposed areas of the skin. Men, older people (>50), and those with a history of increased sun exposure are at higher risk for developing this cancer.
Basal cell carcinoma (BCC) is the most common skin cancer and usually develops in sun-exposed areas of the skin. Men, older people (>50), and those with a history of increased sun exposure are at higher risk for developing this cancer.

Basal cell carcinoma generally does NOT spread to lymph nodes or other parts of the body. There are some genetic syndromes that cause the appearance of multiple BCCs such as Gorlin syndrome, also known as Nevoid basal cell carcinoma syndrome (NBCCS).
There are three main types of BCC:
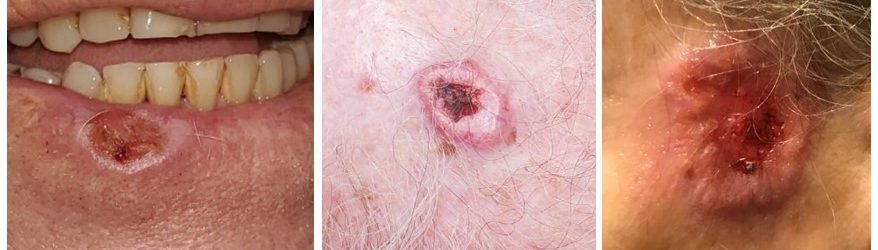
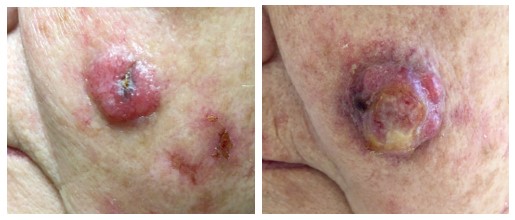
- Nodular is the most common type of BCC in the head and neck. These lesions typically appear as round, flesh-colored nodules with smooth borders. There may also be a rolled edge with central “crater” type appearance associated with crusting, bleeding or ulceration.
- Superficial spreading BCC is the second most common type of BCC. This is a less aggressive subtype and usually appears as a well-defined reddish-scaly plaque or thin patch.
- The morpheaform subtype of BCC is the most aggressive form because its subtle appearance often leads to a delayed diagnosis. These lesions typically have scar-like plaques or smooth, shiny, pink or whitish lesions.

Diagnosis and Work Up: Diagnosis and workup of BCC starts with a skin and lymph node exam. Basal cell carcinomas often have a typical appearance so your doctor may diagnose the cancer by visual exam but a skin biopsy is usually done to confirm the diagnosis. [Jump to Diagnosis of Skin Cancer]. Most of the time, imaging and lab studies are not needed unless the cancer is large or there is other evidence that the cancer may be invading important deeper structures on the face, head, or neck.
Staging: Staging is a process to categorize the cancer by how big it has grown and how far it has spread.
- Stage 1 The tumor is <2 cm in width and has <2 high risk features It may involve the dermis of the skin but does not involve muscle, cartilage or bone and has not spread to lymph nodes or other organs.
- Stage 2 The tumor is > 2 cm in width and does not invade muscle, cartilage or bone and has not spread outside the skin.
- Stage 3 The tumor has grown outside the skin to structures such as muscle, bone, cartilage or lymph nodes that are nearby. It has not spread to distant organs.
- Stage 4 The tumor has spread to distant organs such as brain, or lung or has invaded nerves of the skull base

Treatment and Outcomes: Most basal cell carcinomas are highly curable with surgery alone. This can be done with a surgery to remove it with a surrounding rim of normal tissue, also called a Wide local excision or with MOHS micrographic surgery. Radiation can also be used by itself to treat basal cell carcinoma or added after surgery for higher risk/ stage BCCs. Risk factors for recurrence include large size and other factors that can been seen on histology [when the cancer is examined under the microscope]. Patients with history of radiation and immunosuppression are also at higher risk for recurrence. If surgery is not an option, there are medical treatments available such as Vismodegib.
Surveillance and Survivorship: Once you have developed a BCC, you are at a higher risk of having or developing another one, so please be sure to follow up with your dermatologist to discuss the need for routine full-body skin exams.
Squamous Cell Carcinoma
Article by Alice Lin, MD
 Squamous cell carcinoma (SCC) can occur in other organs of the body but most commonly occurs on the skin. The cancer usually grows slowly but over time can invade deeper tissues and nerves. When it occurs on the skin, SCC is almost always treatable and is seldom life-threatening, especially when it is treated promptly. Squamous cell cancer of the skin is curable with surgery alone 95% of the time.
Squamous cell carcinoma (SCC) can occur in other organs of the body but most commonly occurs on the skin. The cancer usually grows slowly but over time can invade deeper tissues and nerves. When it occurs on the skin, SCC is almost always treatable and is seldom life-threatening, especially when it is treated promptly. Squamous cell cancer of the skin is curable with surgery alone 95% of the time.
Squamous cell carcinoma is more common in people with fair skin and with a history of increased sun exposure and sun-damaged skin. People in this category can develop multiple SCCs. Sometimes, these cancers are preceded by a pre-cancerous growth called Actinic Keratosis (AK).
Diagnosis and Workup: Diagnosis and workup of SCC starts with a skin and lymph node exam. SCCs often have a typical appearance so your doctor may diagnose the cancer by visual exam, but a skin biopsy is usually done to confirm the diagnosis. [Jump to Diagnosis of Skin Cancer]. Most of the time, imaging and lab studies are not needed unless this is a large cancer in a delicate area or there is a concerning finding on physical exam.
Staging: Staging is a process to categorize the cancer by how big it has grown and how far it has spread
- Stage 1: The tumor is smaller or equal to 2cm in greatest dimension and has not spread to lymph nodes or other organs
- Stage 2: The tumor is larger than 2cm, but smaller than or equal to 4cm is greatest dimension. It has not spread to lymph nodes or other organs
- Stage 3: The tumor is larger than 4cm or there is minor bone erosion, involvement of nerves, deep invasion defined as extension beyond the fat underneath the skin or more than 6 millimeters in depth or spread to a single nearby lymph node.
- Stage 4: The tumor invades nearby bone or the skull, many nearby lymph nodes or distant organs such as the brain or lungs
Treatment and Outcomes: Superficial treatments can be used for very superficial or shallow cancers, also called squamous cell carcinoma in situ, or Bowen’s disease.
- Cryotherapy- using a cold liquid or tool to freeze cancer cells
- Photodynamic therapy (PDT)- using light energy to activate a drug that is applied to the area
- Topical medications- Imiquimod and fluorouracil(5-FU)
- Electrodesiccation & Curettage – scraping away the visible tumor with a sharp tool followed by cauterization of the base of the wound with an electric needle.
- If the cancer is more invasive, treatment usually consists of surgery to remove the cancer. This can be done with Mohs micrographic surgery or conventional surgery (WLE). Radiation may be used rarely as primary therapy or added after surgery [See radiation].
- If your cancer returns after it has been treated, this is considered a high-risk squamous cell skin cancer. Other high-risk situations include fast growth, growing deeply, a weakened immune system, a tumor that forms in skin that has been previously damaged by a burn, surgery or radiation and signs of nerve involvement. High risk situations are more likely to require radiation after surgery.
Surveillance and Survivorship: Once you have developed a SCC, you are at a higher risk of having another one, so please be sure to follow up with your doctor and also with your dermatologist to discuss the need for routine full-body skin exams.
Cutaneous Malignant Melanoma
Article by Alice Lin, MD
 Melanocytes are the cells that produce the pigment responsible for the color of your skin and cancer arising from these cells is called Melanoma. Melanoma is more rare than basal cell and squamous cell skin cancer and is considered a more dangerous type of skin cancer as it has a higher risk of spreading to lymph nodes or remote parts of the body. Melanoma can develop from a pre-existing mole or can appear as a new pigmented spot in the skin. Most melanomas are shades of brown or black but some can appear as lighter colors.
Melanocytes are the cells that produce the pigment responsible for the color of your skin and cancer arising from these cells is called Melanoma. Melanoma is more rare than basal cell and squamous cell skin cancer and is considered a more dangerous type of skin cancer as it has a higher risk of spreading to lymph nodes or remote parts of the body. Melanoma can develop from a pre-existing mole or can appear as a new pigmented spot in the skin. Most melanomas are shades of brown or black but some can appear as lighter colors.

Risk Factors: There are several risk factors that increase your risk for melanoma
- Light or fair skin and light hair color
- Genetics/family history: those with a family history of melanoma are more likely to develop melanoma
- Having many moles [nevi] on the skin: Having many moles increases your risk as these moles have the ability to become melanoma. However, most moles never become melanoma.
- Ultraviolet [UV] rays are also linked to melanoma and therefore a history of severe childhood sunburns or increased sun exposure can increase the risk of melanoma.
Diagnosis and Workup: Diagnosing and treating melanoma early and accurately increases the probability of successful treatment. If you have risk factors for melanoma, you should seek a skin exam by a health care professional, but you should also frequently examine your own skin. Knowing if there is a change to a mole is very important information in the diagnosis of melanoma. When looking for melanoma, the following worrisome features can be remembered using the melanoma “ABCDE’s”:
Melanoma ABCDE’s
A is for Asymmetry: look for an irregular shape or two halves of the lesion that are differently shaped
B is for Border: look for irregular borders that are not smooth
C is for Color: look for different colors within the pigmented spot or different shades of color
D is for Diameter: diameter larger than 6 millimeters or a quarter of an inch is concerning
E is for Evolving: look for growths that are changing in size, color or shape. Bleeding or itching are also concerning signs
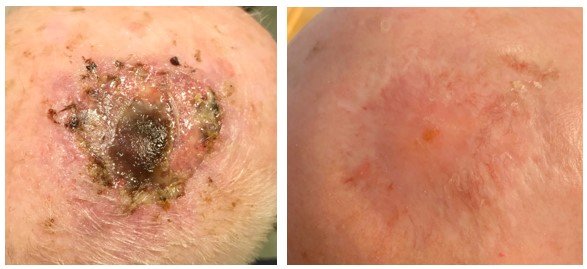
Workup for melanoma starts with a whole body skin exam and lymph node exam and a skin biopsy. The biopsy material may be tested for gene mutations, such as mutation in a gene called “BRAF”. Melanomas with BRAF mutations may respond to certain drugs designed to specifically block the BRAF gene pathway. Early stage melanoma often does not require imaging tests but more advanced melanoma will require imaging in the form of a PET scan, an MRI and/or CT scan. sentinel lymph node biopsy is also recommended for melanoma that is close to or more than 1 mm in thickness. Sentinel lymph node biopsy uses a special injection and imaging to find lymph nodes near the melanoma, where the melanoma cells could potentially travel. The thickness of the melanoma is determined by the skin biopsy. [Jump to sentinel lymph node biopsy]

Staging: Staging is a process to categorize the cancer by how big it has grown and how far it has spread For melanoma, the depth of the tumor and presence of ulceration is important for staging.
- Stage 1: The tumor has a depth of 1.0 mm or less with or without ulceration or is between 1.1-2.0mm without ulceration and has not spread to lymph nodes or other organs
- Stage 2: The tumor is between 1.1-2.0mm with ulceration or greater than 2.0mm with or without ulceration and has not spread to lymph nodes or other organs.
- Stage 3: The tumor has spread to nearby lymph nodes or through lymph channels to separate areas of the skin but has not spread to distant organs
- Stage 4: The tumor has spread to distant areas such as the lungs or brain
Treatment and Outcomes: Treatment of melanoma is generally surgery to remove the melanoma along with a rim of normal tissue around it. The width of this rim is determined by the depth of the melanoma and any other high-risk features. If the sentinel lymph node biopsy was done and showed cancer in the lymph node, removal of the lymph nodes from the neck, also called a neck lymph node dissection or “Neck dissection” with or without removal of lymph nodes from the large saliva gland overlying the jaw, also called a “Parotidectomy” may be considered. Removing the lymph nodes decreases the chance of the melanoma coming back in the head and neck area which is dangerous to all the important structures in the head and neck. After surgery, radiation and/or adjuvant chemotherapy be recommended.
Surveillance and Survivorship: Once you have developed a melanoma, there is a risk the melanoma can come back in the same area, in lymph nodes or other areas of the body. As time goes on, this becomes less likely, but a small risk persists. You are also at increased risk of developing another melanoma. In order to decrease the risk of melanoma, it is important to avoid and/or cover up from the sun, use sunscreen when outside, and avoid tanning beds and UV lamps.
Merkel Cell Carcinoma
Article by Alice Lin, MD
Merkel cell carcinoma [Neuroendocrine carcinoma of the skin] is a rare and aggressive type of skin cancer, but it is becoming more common. It can grow quickly in its local area of the skin and can also spread to lymph nodes and other distant parts of the body such as the lungs, liver, bone or brain. Early diagnosis can be life-saving.
This skin cancer most commonly appears in the head, neck or face and most often develops in older people with a history of a lot of sun exposure. It is also more common in people with a compromised immune system. Merkel cell cancer can look like a sore or a shiny pink, red or purple spot. It can be difficult to spot a merkel cell cancer based on appearance alone.
Accurate and early diagnosis and treatment of Merkel cell cancer increases the probability of success. The process starts with a skin and lymph node exam and a skin biopsy. Once merkel cell cancer is confirmed, a sentinel lymph node biopsy is the best way to determine if the cancer has spread to nearby lymph nodes.
The Positron Emission Tomography scan, or PET scan, has been shown to be very useful for Merkel cell cancer. A PET scan uses radioactive tracers to detect disease in the body,- cancers of a large enough size (usually ~1 cm or larger) can have a bright signal on a PET body scan. Your doctor may also order other types of imaging, such as an ultrasound, CT scan or MRI.
Staging: Staging is a process to categorize the cancer by how big it has grown and how far it has spread.
- Stage 1 The tumor is less than 2 cm in size and has not spread to lymph nodes or distant organs
- Stage 2 The tumor is greater than 2 cm in size but has not spread to lymph nodes or distant organs. It may involve muscle, bone, fascia or cartilage that is underlying the primary tumor
- Stage 3 The tumor spread to lymph nodes
- Stage 4 The tumor has spread to distant areas such as lung, liver, lymph nodes far away from the primary tumor or skin far away from the primary cancer
Treatment and Outcomes: Merkel cell cancer is usually treated with surgery to remove the cancer along with a wide rim of normal tissue around it. The wide rim or margin of normal tissue removed with the cancer decreases the chances of the cancer coming back. However, if the merkel cell cancer is on the face, a wide margin may not be possible or may be aesthetically unfavorable. Smaller margins or MOHS surgery can be considered. If surgery is not possible or desirable, radiation can also be used as primary treatment – this decision should be discussed with the patient’s entire care team (medical oncologist, radiation oncologist, surgeon).
If a sentinel lymph node biopsy shows that cancer has entered the lymph nodes, your doctor will most likely recommend removal of the lymph nodes in the neck. This may also include removal of a portion of the saliva gland called the parotid gland which contains lymph nodes overlying the face. After surgery, radiation is recommended to follow closely afterwards unless the cancer was very small. Radiation is used to treat the area of the cancer and possibly the area of the lymph nodes if the lymph nodes were involved. Chemotherapy can sometimes be used but has not been shown to demonstrate a clear benefit except when the merkel cell cancer has metastasized to distant organs.
If the cancer has spread to distant sites, a clinical trial is preferred. Surgery is usually not recommended and treatment with radiation and or chemotherapy or immunotherapy are the more common options at this point.
Surveillance and Survivorship: After the cancer is treated, merkel cell cancer has a higher risk of coming back in the same area than other skin cancers. It is recommended by the National Comprehensive Cancer Network, NCCN, to follow up with your physician regularly for physical check-ups every 3-6 months for the first two years and every 6-12 months thereafter. Most recurrences happen within the first two years.
Sebaceous Cell Carcinoma
Article by Karen Choi, MD
Sebaceous carcinoma is an extremely rare skin cancer that arises from the sebaceous glands in the skin. These glands are located throughout the surface area of your skin and are responsible for producing the oils, known as sebum, and open onto your hair follicles. Sebaceous cell carcinomas are most commonly found in the head and neck region, especially the eyelids, but can develop anywhere on the body. Sebaceous cell carcinomas are more common in older patients (>40 years old) and Caucasians. The cause of these cancers is unknown and there is no clear link to sun exposure. A small percentage of cases are related to a genetic syndrome called Muir-Torre syndrome.
Diagnosis: Sebaceous cell carcinoma typically presents with a slowly enlarging firm subcutaneous nodule. This should be evaluated promptly by your doctor. Once confirmed, your physician may evaluate the lymph nodes with exam and/or imaging. A sentinel lymph node biopsy and/or surgical removal of lymph nodes [Jump to Neck Dissection] may be recommended by your doctor.
Staging:
Treatment and Outcomes: Treatment of sebaceous cell cancer is generally surgery to remove the cancer along with a wide rim of normal tissue around it. If the sentinel lymph node biopsy was done and was positive, your doctor may recommend removal of the lymph nodes in the face or neck that drain your cancer.. This may also include removal of a portion of the saliva gland called the parotid gland which contains lymph nodes overlying the face. In some cases, patients may require radiation or chemotherapy after surgery.
Surveillance and Survivorship: Sebaceous carcinoma can recur as late as 5-10 years after treatment. Therefore, patients should be followed regularly by their doctor after treatment indefinitely.
*******************************************************************
Diagnosis of Skin Cancers
Skin Biopsy
A skin biopsy is the removal of a small piece of the suspicious appearing area so that it can be examined under the microscope to determine the type of disease and its features. Your doctor will determine if the lesion looks suspicious enough to warrant a biopsy and what type of biopsy is ideal for you.
- Shave biopsy – a biopsy that shaves off the top layer of the skin with a small blade
- Punch biopsy – a small and round tool resembling a cookie cutter is used to remove a cylinder of skin in order to remove a deeper sample that includes all the layers of the skin.
- Excisional biopsy –the entire lesion that is visible to the human eye is removed in one piece with a surgical blade and sent to the lab for analysis.
- Incisional biopsy – a portion of the lesion is removed with a surgical blade and sent to the lab for analysis.
Lymph Node Biopsies
Fine needle aspiration (FNA): A fine needle aspiration is the use of a small hollow needle to extract cells from the lymph nodes. These cells can then be examined under the microscope. The procedure generally causes minimal pain and does not leave a scar but may not provide enough sample to accurately make a clear diagnosis.
Core needle biopsy: A core needle biopsy is the use of a large hollow needle to remove a very thin cylindrical core of sample from the lymph node. The procedure is quick but may cause slightly more temporary discomfort than a fine needle aspiration. This type of biopsy collects a bigger sample and is more accurate than using the smaller needle. This type of biopsy is often carried out using image guidance with an ultrasound or CT scan for more accurate placement of the needle
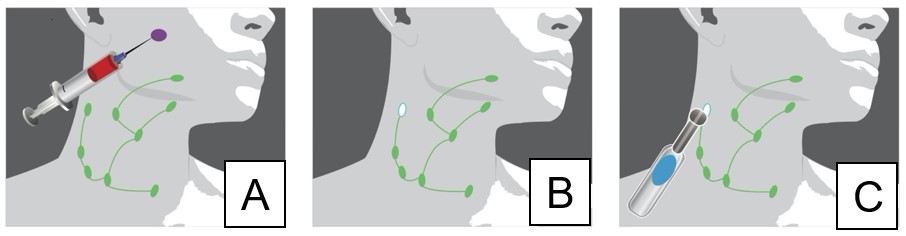
Sentinel lymph node biopsy may be an important part of your treatment for melanoma, merkel cell carcinoma and certain high-risk squamous cell skin cancers. The role of sentinel lymph node biopsy is still evolving for squamous cell skin cancers. This procedure is used to find the first lymph nodes that drain your skin cancer and test those lymph nodes to see if the cancer has spread into the lymph nodes. The procedure begins with injection of a radioactive tracer into the cancer. [A] An imaging exam called lymphoscintogram is then performed to show the location of the sentinel lymph node[s] [B]. The lymph node[s] are then removed by the surgeon and analyzed in the laboratory and tested for cancer [C]. If the lymph nodes are cancer free, the cancer is unlikely to have spread and more invasive lymph node removal procedures are likely not needed. If the lymph nodes do contain cancer, more lymph node surgery, as well as other treatments, may be recommended by your multidisciplinary oncology team (surgeon, oncologist, radiation oncologist).
Treatment
Superficial Treatments
Squamous cell carcinoma in situ or Bowen’s disease can be treated with superficial treatments as these cancers have not invaded past the most superficial layer of the skin, the epidermis. Superficial treatments include
- Cryotherapy- using a cold liquid or tool to freeze cancer cells
- Photodynamic therapy(PDT)- using light energy to activate a drug that is applied to the area
- Topical medications- Imiquimod and fluorouracil(5-FU)
- Electrodesiccation & Curettage – scraping away the visible tumor with a sharp tool followed by cauterization of the base of the wound with an electric needle.
Surgery:
Wide local excision: Traditional surgery, also referred to as a wide local excision (WLE), removes the cancer with a rim of normal tissue around the cancer, called a margin. Having a complete margin removed with the cancer decreases the chances of the cancer coming back. The thickness of the margin is dependent on the type of cancer and the cancer’s features that indicate how aggressive the cancer is. The thickness of the margin may also be selected by your surgeon based on the exact location of the cancer and its proximity to important delicate structures of the face (for example, the eyelids). Surgery can sometimes be performed in the office but if the cancer is large or in a sensitive area, this may need to be done in the operating room with anesthesia.
MOHS micrographic surgery: a technique that allows a specially trained dermatologist or surgeon to remove the least amount of normal tissue possible in the removal of your skin cancer. This is especially advantageous in aesthetically sensitive areas on the face, such as around the eyes, nose, mouth or ears. In MOHS surgery, after all the visible tumor is removed with a scalpel, a thin rim of normal tissue is removed from the wound and checked under the microscope while you are waiting to look for any residual cancer cells. This is a slow process that continues while you wait until the final layer shows no residual cancer cells. This creates the smallest possible wound while still removing all of the cancer cells. After MOHS surgery, the wound is sewn back together, leaving a scar. MOHS is effective for the treatment of basal cell carcinoma and squamous cell carcinoma. The usefulness of MOHS surgery in melanoma, merkel cell carcinoma and sebaceous cell carcinoma is debated.
The Role of MOHS Micrographic Surgery and Standard Surgery Excision [WLE]: For basal cell carcinoma both MOHS and standard surgery [WLE] have very high success rates for treating the cancer. MOHS may allow the cancer to be completely removed while taking a smaller margin, thus leaving a smaller scar. Wide excision is necessary when the basal cell cancer extends to structures deeper than the skin.
For squamous cell carcinomas, MOHS has been shown to have a lower rate of recurrence. However, if the cancer is very large or has invaded deep structures under the skin, MOHS may not be possible and traditional surgery [WLE] would be advised instead.
Neck Dissection: Lymph nodes are small structures that collect and filter material for the lymphatic system (which is a body-wide network drainage system that filters body fluids of infectious foreign particles). The lymphatic system can also collect and filter cancer cells. Therefore, cancer cells can spread to lymph nodes and grow. A Neck Dissection is a surgery to remove the lymph nodes of the neck that may contain cancer cells. This surgery is done under general anesthesia to allow detailed work around the delicate nerves and structures of the neck. A neck dissection attempts to remove all of the lymph nodes in the area of which the cancer has the ability to spread. After a neck dissection, despite the absence of lymph nodes in the specific area of surgery, your lymph generally finds and uses other lymph pathways to move through the neck.
Parotidectomy: The parotid gland is the large saliva gland that lies in front of the ear lobe over the side of the face and overlying the jawbone. This gland makes saliva but also contains lymph nodes. A parotidectomy is removal of part or all of the parotid gland and may be part of the treatment when lymph nodes have to be removed in that area for skin cancer. Your mouth has 800-1000 other saliva glands so you will not miss the saliva made by the parotid gland after it is removed.
The facial nerve runs through the parotid gland and splits the gland into a superficial and a deep lobe. Parotid surgery requires identifying the very thin nerve as it travels through the parotid gland, and the surgeon’s goal is to keep all of the nerve branches safe during parotidectomy. When the parotid or the lymph nodes in the parotid contain cancer, the cancer can grow and invade these nerves, destroying them and thus causing weakness of the face.
Radiation: Radiation therapy is the use of high-energy waves to kill cancer cells. Radiation can be given in several forms such as external beam radiation therapy (EBRT) or directly applied via electronic brachytherapy).
Brachytherapy delivers radiation directly to the cancer via a miniaturized x-ray source. This allows treatment of the cancer without surgery and is useful when surgery is not an option or not desirable. However, brachytherapy only penetrates the skin to a short depth and therefore can only be used for certain small cancers which do not invade deeply.
Patients receiving traditional radiation therapy (EBRT) will need several radiation treatments, and the schedule will depend on the regimen selected by the radiation oncologist. This is often more cumbersome than having surgery or MOHS. Side effects of radiation are temporary and include redness, skin changes, skin breakdown and fatigue. Permanent side effects of radiation are less common, but include an unfavorable appearance of the skin, non-healing ulcers and cataracts if given near the eye. There is also a small risk of cancer recurring in the radiated area and the radiation itself can cause skin cancers to form, usually several years after treatment. Generally, radiation is not as effective as surgery in the primary treatment of skin cancer and the same area should only be treated once with radiation.
Primary
Surgery is usually the best way to treat skin cancers but, in some cases, radiation therapy can be used as the main (primary) treatment and thereby avoid surgery. There can be good results for certain basal cell carcinomas and squamous cell carcinomas. This may also be true for merkel cell cancer but generally surgery is preferred. Radiation is very rarely used as primary treatment for sebaceous cell carcinoma ormelanoma.
Adjuvant
Radiation can also be used as an added treatment after surgery to treat cancer that was not completely removed or to decrease the likelihood of the cancer returning. Radiation is sometimes needed for cancers that have grown into larger nerves or skin cancer that is invading very deeply even if the cancer was entirely removed by surgery.
Systemic Therapy
What is systemic therapy?
Systemic therapy is a medicine that affects the entire body and has the potential to treat cancer cells throughout the body. Most systemic treatments are given by an IV infusion, however some can also be given as a pill.
The most common types of systemic therapies are chemotherapy, immunotherapy, and targeted therapy.
Chemotherapy is a drug therapy that is put into the bloodstream to kill fast-growing cells in your body. Since cancer cells grow more quickly than other cells, these drugs preferentially kill cancer cells over other non-cancerous cells.
Immunotherapy is a drug therapy that can either educate the immune system to recognize and attack a certain type of cancer cell, or enhance the performance of the body’s immune system to fight cancer.
Targeted therapy is a drug therapy that targets specific genes and proteins that regulate the growth and survival of cancer cells. This indirectly kills the cancer cells or slows down its growth.
Chemotherapy has very little effect on skin cancers and is generally only used in the following situations:
- When surgery, radiation, and immunotherapy are not options
- When patients have a metastatic Merkel cell carcinoma and immunotherapy is not available.
- When radiation is being given after surgery, chemotherapy may be given with it to make it more effective.
Immunotherapy is the primary systemic treatment for skin cancers. Immunotherapies are methods that use the patient’s own immune system to kill cancer cells. There are several types of immunotherapy, but the most common group are called “immune checkpoint inhibitors”. These medicines are highly effective for melanoma, Merkel cell carcinoma, and squamous cell carcinoma. This type of treatment is commonly used when the cancer has spread somewhere else in the body and cannot be removed with surgery. These medicines are generally very well tolerated and have less side effects than traditional chemotherapy. Sometimes this medicine may be given after surgery, as well in hopes of decreasing the likelihood of the cancer coming back.
Targeted therapy is currently used for both melanoma and basal cell carcinoma. For melanoma the common target is the BRAF signaling pathway – mutations that cause this genetic pathway to be overactive are present in about 30% of head and neck melanomas. Much like immunotherapy, targeted therapy is typically used for melanoma that has spread somewhere else in the body or after surgery for a high-risk melanoma. The hedgehog inhibitor is a targeted therapy useful for basal cell carcinomas. This can be used for basal cell skin cancers that spread elsewhere in the body but also for cancers that continue to recur after surgery or radiation.
Clinical Trials
article by Kevin Emerick, MD
Clinical trials help determine how effective new treatments are for diseases. Most clinical trials use hundreds or thousands of patients from multiple hospitals and compare two different types of treatments to identify which is best. However, smaller clinical trials are also common, especially for very new treatments. For skin cancers, the majority of large clinical trials have investigated systemic treatments for melanoma. There are a few smaller trials that have also investigated some of the systemic treatments discussed above for Merkel cell carcinoma, squamous cell carcinoma, and basal cell carcinoma.
Thanks to many of the trials done with melanoma patients, the safety and benefits of immunotherapy and targeted therapy treatments are well established. Now, trials are focusing on different timing and dosing to give these medicines in hopes of optimizing the benefits and limiting any side effects. Clinical trials for Merkel cell carcinoma and squamous cell carcinoma in particular are still in the early phases of helping to define how helpful these medicines can be. The small number of studies for both of these diseases show many of these tumors that have metastasized will respond to treatment. Clinical trials are now focused on investigating if these are helpful if given before or after surgical treatments.
Clinical trials are an important way to improve patient care and identify better treatments. Because many skin cancers have shown excellent responses to immunotherapy and some targeted therapies, there are a growing number of strategies being developed to improve skin cancer treatment. Patients with advanced skin cancers may have opportunities to participate in some of these trials. Patients looking for clinical trials can visit the website https://clinicaltrials.gov/ where all trials active in the United States must be registered.
Survivorship
Once you have had skin cancer treatment, you should continue to follow up with your physician to determine the right schedule for routine checks of the area, as well as, the rest of the body for other new skin cancers. [surveillance link] Care should be taken to prevent the return of the cancer and development of more cancers. [prevention link] If you had a high-risk skin cancer removed with surgery, your providers may get a multidisciplinary tumor board opinion on whether further treatment is needed to effectively treat the cancer. A clinical trial may also be available to you. [clinical trial link]
For more information regarding survivorship and considerations after treatment, please follow these AHNS links pertinent to skin cancer:
Skin Cancer Prevention
Article by Mirabelle Sajisevi, MD
Most skin cancers are related to the damaging effects of ultraviolet (UV) radiation from the sun. Therefore, protecting yourself in the following ways can reduce the risk of developing skin cancer:
- Stay in the shade if possible during the hours of 10am to 4pm
- This is important all year round
- Apply broad-spectrum sunscreen to all exposed skin surfaces with sun protection factor (SPF) 30 or higher that provides protection against UVA and UVB rays
- Reapply sunscreen every two hours if outside or when swimming or sweating
- Use sunscreen even on cloudy days and near reflective surfaces like water, sand and snow
- Wear protective clothing including long sleeved shirts, pants, hat and sunglasses
- Tightly woven fabric in darker colors offers the most protection
- A wide brimmed hat that shades the face, ears and neck is ideal
- Avoid tanning beds and sunlamps which emit UV radiation
Surveillance for Skin Cancer (What to do after finishing treatment):
Article by Alice Lin, MD
How often will my doctor see me after my cancer treatment is completed?
Your doctors may examine your skin and lymph nodes following a typical schedule such as every 3-6 months for the first two years and every 6 to 12 months after 2 years. A patient’s particular schedule is unique, so you may be seen more/less frequently:
If your cancer comes back, it usually does so in the first two years. As the time passes further and further from your cancer treatment, you can be more assured that your cancer will not return. However, you are still at risk of developing other skin cancers.
Which doctor should I see?
If your skin cancer was treated by several different doctors or specialties, all of your treating physicians will want to see you after treatment. Depending on your status, your team may elect to alternate visits between physicians. Once more time has passed and the cancer is less likely to return, you will still need to follow up with your dermatologist regularly for whole body skin exams.
What imaging will I require during my surveillance period and when should I get it?
- Imaging after skin cancer treatment is somewhat controversial. There may be some benefit of routine surveillance imaging but in many cases the physical exam may be more informative and accurate. One benefit of routine imaging may be the possibility of catching deep or silent recurrences early and some negatives include increased anxiety, unnecessary radiation exposure and cost. For most skin cancer surveillance, imaging is not beneficial.
- In cases of large skin cancers or metastatic skin cancers, your doctor may order new baseline imaging within 3-6 months after treatment completion but again this may not be necessary. The imaging can be in the form of PET(Positron Emission Tomography) scan, CT (Computed Tomography scan) or MRI (Magnetic resonance imaging) scan depending on the type of primary cancer treatment and your doctor’s judgement.
What other tests should I have done during surveillance?
- You should have a WSE [Whole body skin exam] with your dermatologist or primary care physician every 6-12 months.
- If you have had radiation to the neck area, you should have thyroid hormone testing every 6-12 months.
- If you have had radiation in the vicinity of your mouth and jaw, you should follow up with a dentist for cleanings and evaluations regularly.
When should I call my dermatologist?
- A new bump or scab, new pain or spontaneous bleeding in the skin
When should I call my cancer doctor?
- A bump or scab in the area of your previous cancer
- A new pain or spontaneous bleeding near your scar
- A new lump or mass that you feel in your neck [link to self lymph node exams]
- Unexplained weight loss
Coming Soon! VIDEO for head and neck self lymph node exam
- Self exams: Video head and neck lymph node exam
- Using the soft pads of your fingertips in a gentle circular motion
- (1) feel the area in front of the ear and travel below the ear
- (2) travel towards the back of the ear to the area behind the ear
- (3) travel down the neck and feel for any knots or nodules that are different from one side to the other.
- (4) relax the muscles on the side of the neck that you are examining
- (5) travel down to the collar bone and then towards the back of the neck and continue the exam upwards in the backside of the neck towards the base of your skull